My return to Dr. B – the ob/gyn who helped saved my life from endometrial cancer in 2014.
Month: May 2019
Medical spreadsheets are soooo very sexy!
A brief explanation of my medical spreadsheet and why I have one.
Feeling like fake news
When you can’t see what’s wrong with you the same way you can see a broken bone, or a cut, or even a runny nose, it’s easy to wonder how real it all is. Sometimes my brain tries to tell me that I’m just imagining my health issues.

When things get Golden
How The Golden Girls reminded me of what you need to do to help yourself when you are sick.

By the pricking of my thumbs
A little bit about my current attempts to get a new diabetic monitoring device.

3 for 3 – yay me!
Doc Talk: Last week I had appointments with 3 of my doctors. (I have “doctors” now – aren’t I posh?)
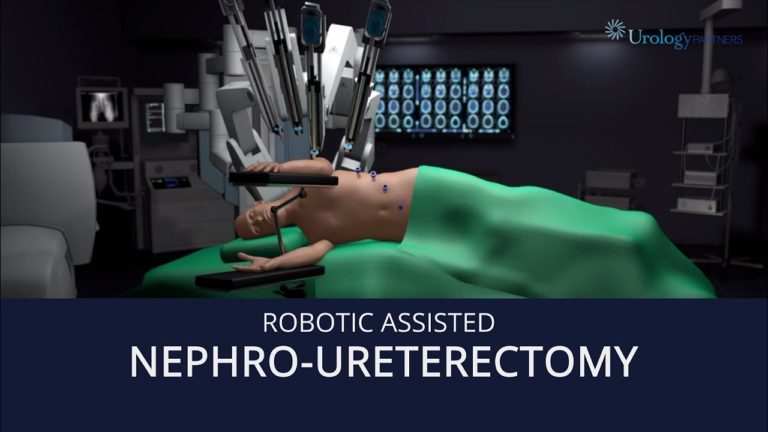
Nephro-ureterectomy (Gesundheit!)
I find out the surgical game plan- we use robots!
Sulphur, Anyone?
Every morning I take 10 different types of pills and 2 injectables. I line them up by size and shape, the smaller ones in pairs, and then begin to work my way down the line. Pop some pills, wash it down with water, repeat. When I get to the bigger ones, I sometimes allow myself…
